Atrial flutter is the second most common arrhythmia after atrial fibrillation. The condition does not have specific symptoms and is difficult to recognize until it worsens.
1. What is atrial flutter? Mechanism of atrial flutter
Atrial flutter is a reentrant arrhythmia characterized by a regular atrial rate. On the electrocardiogram, the intervals between atrial waves are not clear. It is differentiated from atrial tachycardia in that the mechanism of atrial tachycardia is due to increased automaticity of atrial muscle cells or small reentrant circuits in the atrium, which show clear atrial waves (p’) and distinct intervals between those waves. However, the distinction is only relative, as many atypical atrial flutters also present patterns resembling atrial tachycardia.
Atrial flutter ranks second among atrial arrhythmias. Atrial flutter and atrial fibrillation can sometimes occur together in the same patient, at the same time, and on the same electrocardiogram. Unlike atrial fibrillation, atrial flutter rarely lasts more than a few hours or transitions to sinus rhythm; most of the time, it progresses to atrial fibrillation.
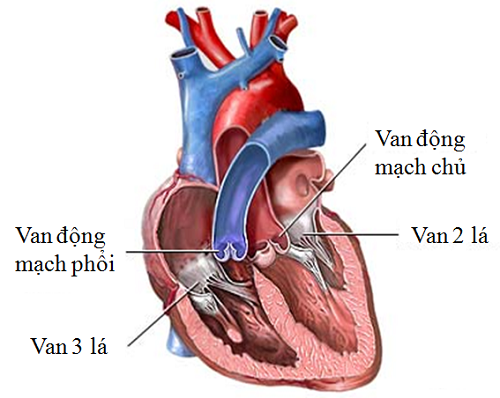
Mechanism: Most cases of atrial flutter are caused by a large reentrant circuit involving a slow conduction pathway between the tricuspid valve and into the right atrium, typically with the reentrant circuit traveling in a clockwise direction.
2. Classification of atrial flutter
2.1. Cavotricuspid isthmus-dependent atrial flutter
Counterclockwise atrial flutter: As previously referred to as typical atrial flutter, it is the most common form of atrial flutter, even in patients who have undergone right atrial surgery to treat congenital heart disease. According to the principles of electrocardiography, the origin of the electrical impulse (negative electrode) will correspond to the negative wave, and the destination of the electrical impulse (positive electrode) will correspond to the positive wave. In this type of atrial flutter, the electrical impulse starts from the negative electrode in the inferior posterior region (corresponding to leads II, III, AVF) and moves clockwise to the positive electrode in the anterior region of the tricuspid valve (corresponding to V1) and then returns to the negative electrode at the interatrial septum (corresponding to V2 to V6), resulting in an ECG pattern with negative F waves in II, III, AVF, positive in V1, and gradually negative towards V6.
Clockwise atrial flutter: This type of atrial flutter has the electrical impulse running from the negative electrode in the anterior region of the tricuspid valve (corresponding to lead V1) and then moves clockwise to the positive electrode in the inferior posterior region (corresponding to DII, III, AVF), resulting in an ECG pattern with positive F waves in DII, III, AVF and negative in V1.
When examining the ECG, one must look at leads II, III, AVF and particularly V1. Especially in many patients, in DII, III, AVF, atrial flutter waves are often difficult to see due to coinciding with the QRS (looking similar to P waves: resembling atrial rhythms), in which case looking at lead V1 will reveal separated F waves. In cases where F waves are not clearly seen in all leads, to better visualize atrial flutter waves, we can perform a parasympathetic test (carotid sinus massage, ocular pressure) or use AV node-blocking drugs (Adenosine, Diltiazem) or perform esophageal ECG to directly access the left atrium. Atrial flutter waves clearly seen in II, III, AVF, and V1 have high specificity (90%) for diagnosing CTI-dependent atrial flutter.
2.2. CTI-independent atrial flutter
CTI-dependent atrial flutter involves a reentrant circuit created by anatomical structures and, as it circles around three leaflets (large circuit), it often has large F waves with a stable cycle. In CTI-independent atrial flutter, the reentrant circuit usually occurs due to functional surfaces and is a smaller circuit, resulting in smaller F waves with oscillating cycles influenced by surrounding electrical impulses; therefore, atrial flutter waves are non-specific.
Right atrial flutter that is CTI-independent (ECG either closely resembles typical atrial flutter or is completely different). This type of flutter often accompanies typical atrial flutter. It is one of the forms of rapid atrial flutter with a frequency < 240 beats/minute and has a clear isoelectric interval between atrial waves.
Left atrial flutter: Due to multiple reentry circuits, atrial flutter waves are often small and the ECG can be variable. This type is often associated with atrial fibrillation. The diverse ECG can be atypical atrial flutter or atrial tachycardia with a cycle < 200 beats/min. It includes:
- Left atrial wall flutter: Caused by a reentry circuit running around the fossa ovalis of the interatrial septum with positive and clear F waves in V1, but low in other leads.
- Mitral valve flutter: The reentry circuit runs around the mitral valve, with an ECG showing low amplitude flutter waves in II, III, AVF and positive in V1, V2.
3. Treatment of atrial flutter
Anticoagulation treatment is similar to that for atrial fibrillation:
Ventricular rate control: In emergency cases, use intravenous route; in non-emergency cases, use oral medications: Adenosine, Verapamil, Diltiazem, Digoxin, beta-blockers. Patients with heart failure should use Digoxin; patients with asthma or COPD should use calcium channel blockers.
Cardioversion and maintenance of sinus rhythm: The pathophysiology of atrial flutter differs from that of atrial fibrillation; the mechanism is due to reentry circuits in the atrial chamber, thus to restore sinus rhythm, several methods are used:
- Create a rhythm to overdrive the atrial frequency to break the reentrant loop
- Ablation of electrical pathways
- Convert the rhythm using synchronized low-energy shocks (50J) with biphasic shocks or by intravenous administration of Ibutilide
- To maintain sinus rhythm and prevent atrial flutter recurrence, Class Ia and Ic medications can be used, especially low-dose Amiodarone at 200mg/day for 5 days a week. Careful consideration is required before using these medications as they may cause arrhythmias.