1. What is diabetic ketoacidotic coma?
1.1 Hyperglycemia
1.2 Ketoacidosis
1.3 Fluid and Electrolyte Disturbance
2. Favorable Factors Causing Ketoacidosis
- Type 1 diabetic patients receiving insulin who suddenly stop insulin, or who are on insulin but have additional favorable factors leading to ketoacidosis-related comas.
- Type 2 diabetic patients who do not have good glucose control along with favorable factors leading to ketoacidosis.
- Trauma
- Stroke
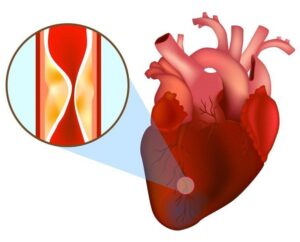
- Myocardial infarction
- Cerebrovascular accident
- Use of drugs with cocaine…
3. Diagnosis of Ketoacidosis in Diabetic Patients
3.1 Clinical Signs and Symptoms of the Disease
- Patients often feel nausea and vomit a lot.
- Feeling thirsty, drinking more water, and urinating more frequently with larger volumes than normal.
- Feeling fatigued, anorexic.
- Changes in vital signs such as rapid heartbeat, hypotension, rapid shallow breathing with Kussmaul breathing pattern.
- Signs of dehydration, dry and hot skin.
- Altered or decreased consciousness such as drowsiness, lethargy, or coma.
- One very specific sign is that the patient’s breath has a ketone odor.
3.2 Signs in laboratory tests
- Blood glucose > 13.9 mmol/L.
- Bicarbonate (plasma) < 15 mEq/L.
- Arterial blood pH < 7.2
- Presence of ketone bodies in the blood and urine.
4. Treatment of ketoacidosis in diabetic patients
4.1 Rehydration
- Hour 1: 0.9% NaCl solution: 15-20 mL/kg (500 mL/m² body surface/hour). If the patient is elderly or has concomitant heart disease, this volume may be lower.
- Hour 2: 0.9% NaCl solution 15 mL/kg. In cases of hypernatremia or congestive heart failure, use 0.45% hypotonic NaCl solution.
- Hour 3: Reduce the infusion rate to 7.5 mL/kg/hour (in adults) or from 2 – 2.5 mL/kg/hour (in young children). The solution used during this stage is usually 0.45% hypotonic NaCl solution.
- Hour 4: Depending on clinical progression, assess the fluid intake and output.
4.2 Use of Insulin
- Initial dose of 0.1-0.15 IU/kg/hour (intravenous injection)
- Then continue intravenous infusion at a dose and rate of 0.1 IU/kg/hour.
- If the patient has no response after 2 – 4 hours of insulin use, and blood glucose does not decrease by 3.9 mmol/L/hour, the infusion dose must be doubled.
- If blood glucose levels < 13.9 mmol/L (250 mg/dL), then the insulin infusion dose should be reduced, and 5% glucose solution (Dextrose 5%) should be added.

- Clinical signs improve.
- Blood pH > 7.3, plasma bicarbonate concentration > 18 mEq/L, electrolyte levels return to normal.
- The patient can eat and has no nausea or vomiting.
- Precipitating factors for the condition (such as infections, trauma, etc.) have been well-managed.
- When switching to subcutaneous injections, intermediate-acting insulin should be used, and the dosage of insulin should depend on blood glucose levels.
4.3 Potassium Replacement
A common electrolyte disorder in patients with ketoacidosis is hypokalemia (incidence 50%). The cause is potassium loss through the kidneys (due to osmotic diuresis, due to loss of reabsorption ability) or due to vomiting, diarrhea, etc. Consider the following factors before proceeding with potassium replacement:
- Does the patient have kidney dysfunction? If the patient urinates ≥ 60ml/hour in the first hour, kidney function is still good.
- What is the current potassium level?
- Monitor the electrocardiogram.
Indications for potassium replacement:
- Serum potassium > 5.5 mmol/L: Do not administer potassium.
- Serum potassium from 3.5 to 5.5 mmol/L: replace with 20 mmol K+/liter of infusion.
- Serum potassium < 3.5 mmol/L: replace with 40 mmol K+/liter of infusion.
- Absolutely do not use intravenous insulin if potassium levels are below 3.3 mmol/L.
5. Considerations in the treatment of diabetic ketoacidosis in patients with diabetes
- It is essential to identify and treat the precipitating factors of diabetic ketoacidosis in patients with diabetes such as trauma, stress, infections…
- Patients need comprehensive care, especially when in a coma.
- Recurrence of diabetic ketoacidosis has a much worse prognosis.
- Cerebral edema and even death can occur. To ensure safety, blood glucose levels should be maintained around 11.1 mmol/L (200 mg/dL) during the first 12-24 hours.
- Nausea and vomiting can cause food aspiration, potentially leading to aspiration pneumonia.
- Hypoglycemia may occur. To prevent this, blood glucose should be maintained at 11.1 mmol/L – 13.9 mmol/L.
- Replacement fluids (especially isotonic saline) may worsen congestive heart failure.
6. Prevention of diabetic ketoacidosis in patients with diabetes
- Patients need to be instructed on how to self-monitor their blood glucose levels.
- Seek medical attention immediately if abnormal signs occur such as nausea, fever, abdominal pain, diarrhea, or high blood glucose levels… or if another condition such as infection, trauma, or pregnancy arises.
- Adhere to treatment, do not reduce insulin dosage independently, or discontinue medication even when experiencing another illness.

