Autologous bone marrow mononuclear cell (BM MNC) transplantation can improve motor function and reduce muscle spasms in children affected by intracranial hemorrhage during the neonatal period.
1. The role of bone marrow mononuclear cell transplantation in treatment
- Intracranial hemorrhage (ICH) occurring in newborns is a serious condition, especially in preterm infants (before 37 weeks of gestation, particularly before 32 or 28 weeks of gestation), leading to high morbidity and mortality rates. Among them, intraventricular hemorrhage (IVH) is the most common form of intracranial hemorrhage in preterm infants, mainly occurring when born before 32 weeks of gestation.
- Causes and circumstances leading to intracranial hemorrhage in newborns:
+ There are many risk factors associated with intraventricular hemorrhage such as premature gestational age, low birth weight (under 2.5 kg), uterine infections in pregnant women, events occurring during normal delivery, pneumothorax, lack of oxygen, hypertension, seizures, and patent ductus arteriosus (a congenital heart condition occurring when the ductus arteriosus does not close).
+ Brain hemorrhage can occur not only in preterm infants but also in full-term infants who suffer from brain injuries, vascular malformations, vitamin K deficiency, and various other conditions such as asphyxia during labor and delivery. The causes of brain hemorrhage in newborns are primarily due to obstetric interventions, especially in difficult delivery cases that require assisted birth methods such as vacuum extraction and forceps.
+ Brain hemorrhage can cause immediate damage or later complications for the brain. Hematomas can have severe effects: increased intracranial pressure, reduced cerebral blood flow, release of inflammatory cytokines and free radicals leading to ischemia and lack of oxygen in brain tissue, white matter damage, and white matter necrosis. These effects can lead to many severe neurological sequelae such as cerebral palsy, seizures, cognitive impairment, hydrocephalus, and even death.
- Methods:
+ Traditional treatment methods for neurological sequelae following brain hemorrhage in newborns have many limitations. Recently, stem cell transplantation has been applied to improve neurological impacts in children, yielding promising results.
+ Mononuclear cell transplantation from bone marrow (Bone Marrow Mono-nuclear Cells – BM MNCs) is a very new therapy in the world for treating neurological sequelae. Mononuclear cells are extracted from bone marrow blood, and then infused into the patient’s body via the spinal cord. The mass of mononuclear cells will follow the circulation of cerebrospinal fluid to the brain. Here, these cells help in angiogenesis, forming substances with anti-inflammatory functions, and stimulating neural stem cells in the proliferative area to differentiate, thereby restoring the damaged brain region.
+ To assess the condition of patients after mononuclear cell transplantation, the applied criteria include: the Gross Motor Function Classification System (GMFCS), motor function and muscle tone assessed by the Gross Motor Function Measure – 88 points (GMFM-88), and the modified Ashworth scale (to assess muscle spasticity).
2. Some treatment results at Vinmec Times City Hospital
Some typical clinical cases of autologous mononuclear cell transplantation from bone marrow to improve neurological sequelae in children affected by intracerebral hemorrhage during the neonatal period:
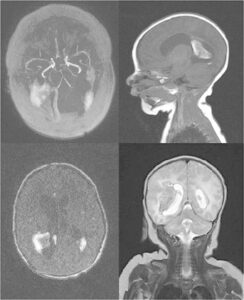
- The boy underwent a cesarean section at week 40 due to prolonged labor. His birth weight was 2.9 kg. He experienced asphyxia immediately after birth, and a brain hemorrhage was detected one day later.
- At 14 months old, the boy was diagnosed with severe cerebral palsy (GMFCS level 5 – the highest level of the gross motor function classification system for children with cerebral palsy) with manifestations including: intellectual disability, hemiplegia, poor motor ability, muscle spasms, Achilles tendon shortening, dysphagia, ability to sit when propped up, but unable to crawl or stand. His vision was poor, as he could only distinguish between light and dark at a very close distance.
- The patient underwent four mononuclear cell transplants from bone marrow at the ages of 14, 17, 24, and 39 months without any adverse events. After treatment, motor ability and muscle tone improved positively (Figure 1). The patient was able to sit and crawl just 3 months after the first transplant, stand while holding onto furniture 10 months after the mononuclear cell transplant, and walk with assistance 25 months after the first transplant. Muscle stiffness reduced from level 2 to 1 on the modified Ashworth scale. Dysphagia disappeared in the 10th month after the first transplant. Vision significantly improved as the patient could recognize and identify light from a mobile phone or other devices and locate desired objects.

- The baby boy was born via emergency cesarean section at 32 weeks of gestation due to oligohydramnios and chorioamnionitis. The birth weight was 1.8 kg. The baby experienced asphyxia at birth and cerebral hemorrhage diagnosed one day after birth. Ventriculoperitoneal shunting was performed at 2 months of age due to hydrocephalus. Motor abilities were limited, and cerebral palsy was confirmed at 9 months of age.
- At 47 months old, the cerebral palsy was classified as severe (GMFCS level 5) with manifestations: intellectual disability, hemiplegia, poor gross and fine motor skills, weak head and neck control, muscle spasticity, arm stiffness, wrist deformity, ankle contractures, and dysphagia. The boy could roll over but could not sit upright. Seizures occurred 1-2 times per week and required the use of antiepileptic medication.
- The patient underwent 3 mononuclear cell transplants from bone marrow at 47, 53, and 59 months of age without any adverse events occurring. After treatment with this method, improvements in gross and fine motor skills were noted 6 months after the first transplant: able to sit steadily when leaning against the wall and using furniture to stand up. Gross motor function continued to improve significantly after 22 months from the first transplant: able to stand independently without support, walk without assistance, or walk using a wheeled walker. Muscle tone decreased, as evidenced by improved results on the modified Ashworth scale, reducing from level 4 to 2. Arm stiffness, wrist deformity, and Achilles tendon shortening all improved. Swallowing difficulties gradually disappeared, allowing the patient to eat solid food (such as rice, etc.). After the transplant, the dosage of anti-seizure medication was gradually reduced and stopped completely after 22 months without any seizures occurring.
- The baby boy underwent a cesarean section at 42 weeks of gestation due to prolonged labor. His birth weight was 3.3 kg. At 33 days old, the baby presented with cyanosis, coma, and was diagnosed with intracranial hemorrhage. Surgery was performed to remove the hematoma.
- At 15 months old, the boy was diagnosed with cerebral palsy at GMFCS level 2 with symptoms: right hemiplegia, poor fine motor function in the right hand, muscle spasticity, spasticity in the right arm, deformities in the hand and wrist, a gait with knee jerks, can stand while holding onto furniture, but cannot walk independently.
- The patient received a single-unit mesenchymal stem cell transplant from bone marrow at 15 months of age without any adverse events. Six months post-transplant, motor function and muscle spasticity showed significant improvement: he could walk, jump, and crawl up stairs without assistance; the spasticity in the right arm had improved; there were no longer any deformities in the hand, wrist, and the knee-jerk gait had resolved.
- A baby boy was delivered by cesarean section at 40 weeks gestation due to placenta previa (the placenta partially or completely covering the cervix). The birth weight was 2.9 kg. At 28 days old, the baby experienced severe vomiting, cyanosis, and coma. A diagnosis of intracranial hemorrhage was made, and it was treated with medication for 20 days without surgical intervention.
- At 68 months old, the boy was diagnosed with cerebral palsy at GMFCS level 4 with symptoms including intellectual disability, hemiplegia, poor fine motor skills, muscle spasticity, knee stiffness, a gait with knee jerks, Achilles tendon contracture, arm spasticity, hand and wrist deformities. He was able to sit without assistance but could not crawl or stand. The patient underwent two mononuclear cell transplants from bone marrow at 68 and 74 months old, without any adverse events. Six months after the first transplant, gross motor function improved: he was able to walk while holding onto objects and could walk with someone holding his hand. Fourteen months after the stem cell transplant, the boy could stand without support and walk when assisted; improvements were noted in his Achilles tendon contracture, knee stiffness, gait with knee jerks, and a reduction in muscle spasticity (from level 4 to level 2 on the modified Ashworth scale).